Struggling with infertility or getting pregnant after miscarriage? This is part of a series of guest posts written by women who got pregnant after loss or infertility. Each post will focus on a special natural fertility or wellness tool that boosted the author’s health, happiness, and fertility on their journey!
This is a guest post by Dr. Sarah Mathis, a board-certified physician in Family Medicine with a passion for hormonal health, fertility, and gut health. She herself struggled with “unexplained” infertility, recurrent miscarriage, leaky gut, and food intolerances. After finding my blog and several other resources, she was able to heal from within and become healthier, happier, and ultimately- pregnant! She pursued her doctorate in osteopathic medicine and is now a functional medicine expert passionate about gently and naturally balancing hormones to boost fertility. This post is specifically about identifying if you may have low progesterone and natural ways to boost progesterone.

Table of Contents
Sarah’s Low Progesterone First Trimester Recurrent Miscarriage Story
I was sitting alone in a dark room with only the faint glow from the ultrasound screen in front of me when I heard the 4 worst words in the world: “There is no heartbeat”.
My body froze and I went pale.
I had gone in for a routine early scan since I had a previous history of miscarriage, but I was not prepared to have this outcome.
Why did I keep having all these miscarriages?
My OBGYN wouldn’t test me for anything because I’d had a previously healthy pregnancy.
I walked out of that appointment still in a daze. And as a physician who is always looking for a cause, I started to search my brain after the initial shock and despair wore off.
I thought back to what I had done differently with my first successful pregnancy.
I was already eating gluten free. I started doing fertility yoga and I cut out HIIT , started following Anna’s dietary recommendations, started praying and getting daily sunshine . . . Yet this time, one thing was different . . .
It was progesterone.
When I finally had my successful second pregnancy, I took a progesterone supplement starting the day I found out I was pregnant. I took it daily with guidance from my functional medicine practitioner until I was 15 weeks pregnant.

How I Figured Out I Had Low Progesterone
Looking back, I should’ve noticed progesterone was my culprit in my infertility struggles. Here are all the symptoms of low progesterone that I experienced but didn’t realize what was going on:
- My luteal phase (after ovulation) was always short, usually less than 10 days. I had a luteal phase defect!
- I experienced insomnia after I ovulated and had significant mood swings and bloating.
- And if I didn’t eat RIGHT NOW, I would spiral into dizziness and lightheadedness from my low blood sugar.
I started going into the rabbit hole of internet research where I searched EVERY possible cause for my miscarriages. FINALLY, I found a page about progesterone and a it was like a lightbulb went off!
I searched how to find out about progesterone testing. At first, I went to my OBGYN, but she was not helpful. After I had my first miscarriage, she just said “these things happen” and that I didn’t need any testing. I asked her about progesterone and she dismissed me and my concerns. She told me I didn’t need it and I was fine as long as I had normal cycles.
I continued my research, looking into who could test and prescribe me the progesterone I knew I so desperately needed. Mind you, I was also suffering from severe gut issues like bloating, numerous food intolerances, sudden weight gain, and extreme exhaustion.
All of these symptoms help lead me to discover functional medicine: treating the root cause of your symptoms versus sticking a bandaid on your concerns and symptoms.
So I again put on my research cap and I found a local functional medicine provider who I felt could help me.

How Functional Medicine Helped Me Get Pregnant with Low Progesterone and Recurrent Miscarriage
And she did. She FINALLY tested all of my hormones and found my progesterone level was in the SINGLE DIGITS. I was not making nearly enough progesterone to support my cycle, let alone a pregnancy!
I started specific supplementation that next cycle. And then the magic happened. After following Anna’s protocol to a T and my supplementation as guided by my functional medicine practitioner, I conceived a healthy baby. Thanks to taking the progesterone, I carried her to full term and now she is a lively and spirited 4 year old.
Sixteen months later, I was blessed again with a surprise pregnancy! Thanks to all the work I did to support myself throughout my pregnancy and postpartum as well, my body healed to have a surprise pregnancy while I was still nursing my baby to once again have another healthy, full term baby. All thanks to progesterone to support me in that first trimester.
Does Progesterone Help Prevent Early Miscarriage?
In my experience, working as a functional health consultant who specializes in infertility and hormonal imbalance, I have found a similar experience of low progesterone in many women who experienced multiple miscarriages, mainly missed miscarriages, in the first trimester.
Oftentimes, they have not been told anything is wrong. Some women had testing done, but often women come to me concerned their progesterone is low, even if it is in “normal range.”
The Role of Progesterone in Repeated Early Miscarriage
The fact is that progesterone helps prevent recurrent miscarriage. Some early miscarriages are due to low progesterone levels. In fact studies show that the higher your number of previous miscarriages, the more likely you are to benefit from progesterone therapy. In fact, the more complicated your pregnancy or past losses, the more likely progesterone may help you. The PRISM trial, which was a large, high-quality, multicenter, placebo-controlled trial that targeted women with unexplained recurrent miscarriages, found that the greatest beneficiaries of progesterone supplementation were women with three or more previous miscarriages and current pregnancy bleeding.
A note from Anna: In my second successful pregnancy I met those criteria- 3 or more losses, and current pregnancy bleeding, and I supplemented with vaginal micronized progesterone as prescribed by my reproductive endocrinologist, and had a healthy baby girl. Read my story of trying for my second child after infertility here!
But, here’s the best news- there are natural ways to boost your body’s on progesterone production!
Let’s back up to the beginning.
By they way, I’m so sorry if you’ve suffered from repeated miscarriage. Please check out Anna’s post on recovering emotionally after miscarriage.

What exactly is progesterone?
Progesterone is one of women’s essential hormones that starts to rise after ovulation to help your body support the fertilized egg as it makes its way towards your uterus. It helps the embryo continue to grow after implantation. Progesterone levels rise and peak during the middle of your luteal phase (the part of your menstrual cycle after ovulation before you menstruate again). If you are pregnant, it should continue to rise as your body creates the previously mentioned corpus luteum, the cyst that is on your ovary after you ovulate that secretes progesterone until your placenta is formed. If you pregnancy occurs, your progesterone levels start to fall and menstruation occurs.
Essentially, it is the hormone that gives life. It supports and maintains pregnancy. And many women, especially those of us trying to conceive who have had multiple miscarriages, have a lower level than we need to support a healthy pregnancy. (PMID: 32644386)
However, sometimes women have low progesterone despite being able to get pregnant. This often occurs with many early missed/first trimester miscarriages, especially if you continue to have recurrent miscarriages with a full workup that does not reveal any other concerns (ex: autoimmune, thyroid, clotting issues, structural issues).
Why is the hormone progesterone so low nowadays?
There are many reasons so many modern women have such low progesterone. Our lifestyle and the foods we eat all play a major role in our progesterone levels. Some of the most common causes can be from obesity, chronic stress and poor diet. Other causes for low progesterone include: hypothyroidism (when your thyroid is not producing enough hormones), hyperprolactinemia (elevated prolactin), low cholesterol, and if you have PCOS or other ovulation issues as well as increased cortisol levels.
Also, after women turn 35, our progesterone levels start to naturally decline as we start approaching perimenopause. Our bodies’ fertility starts to decrease around this time, making it harder to conceive and maintain a healthy pregnancy without enough proper care and preparation for our body.

Why is this so controversial?
Oftentimes, most OBGYNs will state that the evidence is “inconclusive” and the research shows that it “doesn’t support any evidence of increased live birth or decreased miscarriage,” at least with oral supplementation. In the past, the studies done had been smaller, lacked a placebo group, and hadn’t had strong enough confidence intervals to convince gynecologists that progesterone therapy was appropriate for preventing miscarriage, or even after recurrent pregnancy loss.
However, the fact is vaginal micronized progesterone may increase the live birth rate for women with a history of one or more previous miscarriage and early pregnancy bleeding, as seen in this study. (PMID: 33872382) We now have larger, well-developed studies, that include a progesterone group and a placebo group and that show the benefits of progesterone therapy.
Additionally, women with endometriosis related infertility may benefit from progesterone as well. Studies have shown that women who experience endometriosis may be partially resistant to progesterone working on the endometrium (uterine lining that supports pregnancy). This is in part due to an inflammatory reaction that is occurring due to the endometriosis. Women with endometriosis may benefit from progesterone supplementation to help with conceiving as well, as seen in this study. (PMID: 34681696)
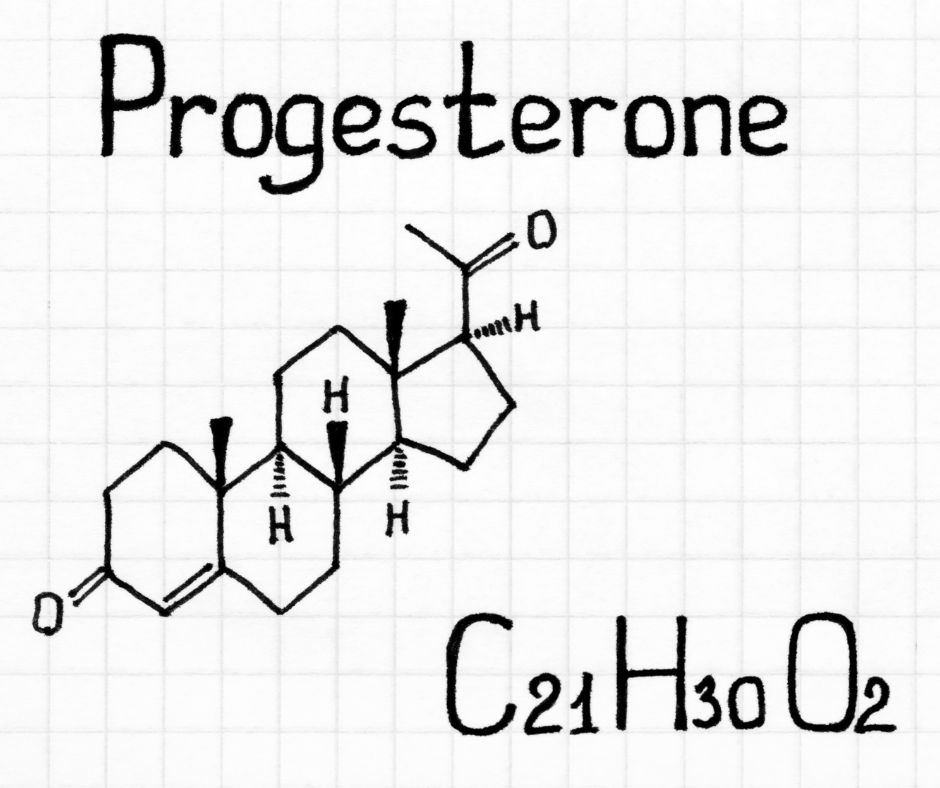
What are the symptoms of low progesterone?
- Low libido
- Hot flashes and night sweats (especially in the second half of your cycle)
- Migraines/headaches
- Depression, anxiety, mood changes
- Insomnia
- Absence of menstrual cycle/irregular menstrual cycle
- Sore breasts (especially in second half of menstrual cycle)
- Low blood sugar
- Spotting between periods
- Vaginal dryness
- Short menstrual periods (shorter than 24 days long)
If you don’t have enough progesterone, you may wind up having estrogen dominance. This can lead to symptoms like:
- Irregular periods
- Mood swings
- Anxiety
- Weight gain
- Bloating
- Low Libido
- Fibrocystic lumps in your breasts
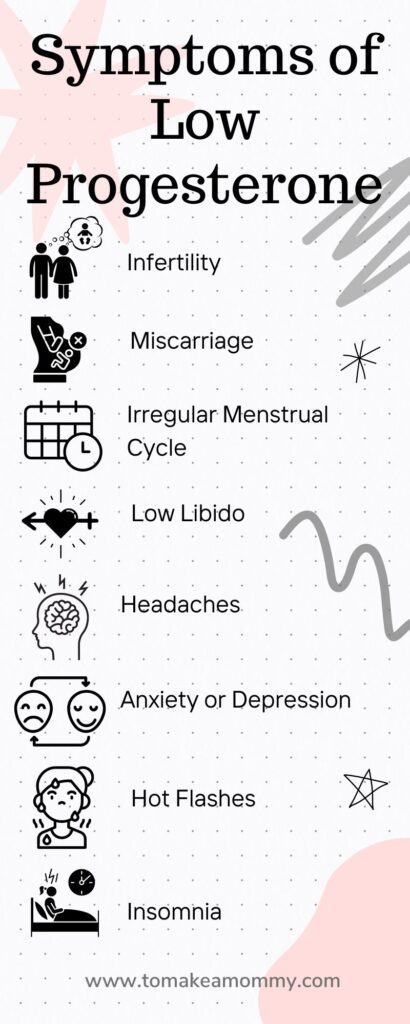
How to tell if you have low progesterone?
Your doctor may order a 21 day blood serum progesterone test. This means on day 21 of your cycle, or around seven days after you ovulate, you will have a blood draw to determine your progesterone level. Remember that day 21 is when progesterone peaks if you have a 28-day cycle. BUT, of course, less than 20% of women have a perfect 28 day cycle, and you’re even less likely to if you have low progesterone!
So, testing on day 21 may not be an accurate gauge of your progesterone levels. So, unless you get your blood tested for several days in a row, you might not get the right levels.
The good news is that there are several at-home progesterone tests that allow you to test urine for Pregnanediol Glucuronide, commonly referred to as PdG, which is the metabolized form of progesterone. levels for several days in a row. This can help you confirm if you ovulated, and help you track amounts over time to see if their are patterns, or if your PdG levels are improving.
At home tests for progesterone as Urinary PdG (pregnanediol-3-glucuronide)
I am aware of two products currently on the market that allow you to test and receive a numeric value of PdG in urine (verses the Proovtest which just confirms ovulation).
Mira-Testing PdG with Mira requires the Mira Analyzer, Mira app, and Confirm Wands. First, you must use a Confirm Wand to take a urine sample. Then, insert the wand into the analyzer and your numeric PdG results will be displayed. You can then use the Mira app to keep track of all of your PdG test results over time. Mira Fertility Max Wands track luteinizing hormone, estrogen, and progesterone at once (LH + E3G + PdG), or you can use Confirm Wands which just track PDG. Mira also makes wands that test FSH! Use code ANNA20 to receive 20% off your order!
Inito– Testing PdG with Inito requires the Inito device, an iPhone, the attachment clip, and testing strips. The actual values of all hormones, including PdG are displaced in the App on your phone. You can use the app to keep track of your hormone results over time! Inito measures Estrogen, LH, & Progesterone metabolite PdG on a single test strip. Use code TMAM15 for 15% off!
Technically measuring at-home urinary progesterone has only been approved for confirming ovulation. But with the Mira and Inito, you will receive numerical results over several days, which can give you insight into cycle to cycle comparison, i.e., if you are improving your progesterone levels.
Understanding Your Progesterone Testing Results
After getting your blood serum progesterone tested, if your progesterone level is less than 5ng/ml, this is considered abnormal. A healthy level in the first trimester is considered by standard laboratory testing to be 11-44ng/ml.
However, in some women, this level may not be optimal for their body’s needs to support a healthy pregnancy. In other words even if you fall in the “normal” progesterone range, you may not be in the “optimal” range. This was my case as well.
I personally had functional medicine hormone testing, which detects all the hormones in a woman’s cycle to determine if there are any problems with the metabolites of progesterone. This shows where in the pathway we need to work on to start to heal. Additionally I run GI maps, full thyroid panels and other various testing that is specific to my client. Oftentimes, a lot of causes for low progesterone start in the gut or due to poor thyroid function.
Please note, there is not a standard level established for urinary PgD.
How can I naturally increase my progesterone levels?
While women often go straight to wanting to just take progesterone supplements, there are non-pharmaceutical approaches to improving the progesterone level as well.
In addition to supplementation, we can support our progesterone levels with multiple different lifestyle and nutritional changes. The three main ways you can boost progesterone levels naturally are by 1) Reducing stress, 2) Eating a progesterone-friendly diet and reducing excess body fat, and 3) Avoiding unhealthy foods and toxins that can unbalance your hormones.
The best thing you can do to support your progesterone level is stress reduction and decreasing any stress in your life, even before addressing nutrition and supplements sometimes.

Reducing Stress for Progesterone Production
There are many ways to reduce stress, and here are some of my favorites.
- Saying no to things you would usually do for others but you know do not benefit you
- Simplifying your life and schedule in general
- Self care, like taking epsom salt baths at night, quiet reading
- Meditation, visualization, and breathwork daily
- Going to sleep before 10pm
- Cutting out alcohol and caffeine (which you already should be doing if you’re following Anna’s advice!)
- Fertility yoga
- Start a Gratitude Practice
- Get Acupuncture
And I get it, I know these things are so much easier to say than to do, but to be honest, if you aren’t taking the time to work on your mind and stress, then you can eat perfectly and take the perfect supplements, but you won’t get the baby you hope for. Stress is the antithesis of healthy pregnancy. It is time to already think of YOURSELF as pregnant in order to visualize that baby in your arms.
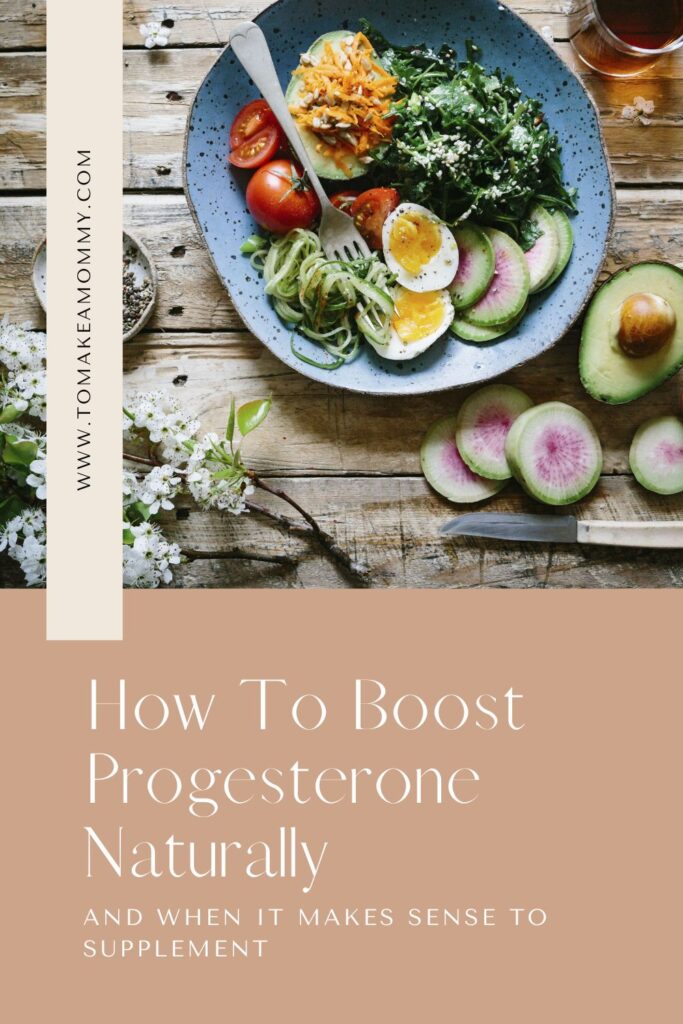
Fertility Foods that Boost Progesterone
However, it is important to still make sure you are supporting your body in addition to your mind. Here are some of my favorite vitamins and minerals that increase progesterone levels and the fertility foods that contain them!
1. Fiber
Fiber helps to flush out excess estrogen to make progesterone levels work more efficiently. Your body absorbs estrogen from food you eat, so the longer food sits in your digestive tract, the more time it has to absorb the estrogen. Improving your bowel movements will decrease the amount of estrogen in your digestive system. Making sure you have around 25-35g of fiber per day.
Some great fertility-friendly, high-fiber foods are:
- Oats
- Flaxseed
- Quinoa
- Fruits
- Vegetables
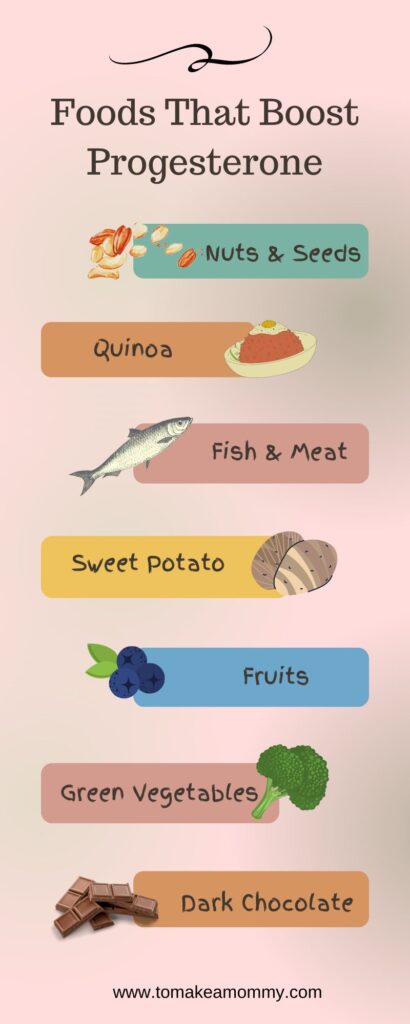
2. Zinc
Zinc is a mineral that is essential in the production of progesterone by increasing Follicle Stimulating Hormone (FSH), that is needed to cause ovulation, which in turn leads to increasing progesterone levels.
Fertility Foods that are high in Zinc include:
- Lean beef
- Seafood
- Pumpkin and squash
- Nuts
3. Vitamin B6
Vitamin B6 has been shown to improve progesterone levels and it is in prenatal vitamins. Women who have therapeutic Vitamin B6 levels have 50% reduction in early pregnancy loss, as seen in this study. (PMID: 17478435)
Here are fertility foods that are high in B6:
- Sunflower seeds
- Sesame seeds
- Chickpeas
- Fish
- Turkey
- Dried fruit
4. Magnesium
Magnesium is so important for many functions, but one of it’s roles in hormone regulation is as a nutrient that increases progesterone levels. It not only also helps the pituitary gland stimulate FSH like Vitamin B6, but it also helps produce Luteinizing Hormone (LH) and Thyroid Stimulating Hormone (TSH) that leads to producing estrogen and boost progesterone.
Foods that are great sources of magnesium are:
- Spinach
- Fish
- Dark chocolate
- Whole grains
- Nuts and seeds
5. Vitamin C
Research has shown that women who consume and take supplemental vitamin C increased their progesterone levels significantly, as seen in this study. (PMID: 12909517)
Some foods high in vitamin C are:
- Yellow peppers
- Oranges
- Broccoli
- Kiwi
- Kale
6. L-arginine
L-arginine is an amino acid that is found in high protein foods to produce nitric acid that aids in increasing blood flow. Nitric acid opens up blood vessels to get more blood flow to areas. More blood flow to your uterus= more likely to grow a healthy baby! Additionally, L-arginine can help thicken endometrial lining.
Some great food sources of L-arginine are:
- Lentils
- Salmon
- Pumpkin seeds
- Chicken
- Pork
- Lean beef
7. Sweet Potatoes/Yams
Oftentimes you will see wild yams as a natural ingredient in progesterone cream. This is a super food that will help with improving your progesterone. However, I do not recommend excessive yam consumption when you have a overlying diagnosis of PCOS, this is why I recommend working with a professional who can help with management of your health concerns.

Avoiding Toxins and Unhealthy Foods that Lower Progesterone
Following Anna’s fertility guidelines (here are her top ten tips) or going all out and doing her list of 79 Things will for sure help you balance your hormones.
Try to eliminate or reduce your exposure to plastic, phthalates, BPA, and other hormone-affecting toxins as much as possible.
See all posts on non-toxic living for fertility.

Foods to Avoid that Can Lead to Estrogen Dominance
- Heavily Processed Food, Food with harmful chemicals, pesticides or added hormones
- Alcohol
- Caffeine
Seed Cycling to Balance Hormones
Although there isn’t a lot of evidence that seed cycling can assist in increasing progesterone and balancing hormones, it is a gentle practice that many women find helpful.
Read all about seed cycling to balance hormones and increase fertility here!
When will you see a change?
Unfortunately, hormones do not act to change overnight. If you are consistent with these changes, you should start to notice a significant change in your cycles in 3-6 months.
If you feel overwhelmed with everything I talked about and don’t know where to start, I’m here to support you!
I see clients virtually 1:1 to support your hormones and bring their hormones and fertility back into alignment through a comprehensive Gut-Hormone Reset program so you can conceive the baby you have been dreaming about! I work with women to cycle sync their nutrition, supplements, exercise and lifestyle habits to make sure you have the most amazing cycles to get pregnant quickly!
I have worked with women to improve their cycles and fertility and I am here to help you too!
It is tough going through your fertility journey alone. It feels frightening and hopeless at times, and I’m here for you through the good and the bad to support you on your goal to getting pregnant and having a healthy baby!
Did you love the nerdiness of this post? Don’t miss these:
- Evidence-Based Tips for Boosting Implantation during the Luteal Phase
- Evidence-Based Sex Tips for Trying to Conceive
- Tracking Macros: Diet Science for Increasing Fertility & Egg Quality
- How CoQ10 Improves Egg Health in Age-Related Infertility
- The Best Prenatals of 2023 for Pregnancy + Trying to Conceive
Want to get pregnant fast?
Love lists? Me too. Grab my 79 Things I did to transform my life and get pregnant in less than 3 months after 2 years of infertility and miscarriages! Totally free!
Dr. Sarah Mathis is a board certified physician in Family Medicine with a passion for hormonal health, fertility and gut health. After her own journey with PCOS, hypothyroidism, recurrent miscarriage, leaky gut, food intolerances, and unexplained fertility, she pursued her doctorate in osteopathic medicine to serve other women who are trying to conceive. She helps high performing women balance their hormones, optimize gut function, boost their fertility, and get pregnant naturally.


After being dismissed by my obgyn when questioning what’s causing my anovulation, I began doing my own research. They essentially laughed when I mentioned the holistic route I wanted to pursue to understand the underlying issues. It’s disheartening to be treated like just another number and even worst, bothersome, when speaking to some medical professionals. This article was very well written and helpful to know I’m not alone in the search for the answer.
I’m so glad you enjoyed the article!! Gaslighting by the docs is real and awful. You are not alone!!
Thank you so much for the work you do. I have found your articles so helpful in my journey to conceive. This article mentions that progesterone blood serum below 5 around 7 days after ovulation is abnormal. How does that translate to the metabolized urine amount? I’m using Inito to check my progesterone during my luteal phase (which is just 10 days currently) but I can’t find any information about what is optimal and what is abnormal for PDG urine tests? I just find blood test amounts.
Oh good question! Are you following Dr. Mathis (who wrote the article) on Instagram? Might be worth sending her a DM!